FAQs: Malaria and antimalarials
- How do you get malaria?
- Do all mosquitoes transmit malaria?
- Are malaria mosquitoes active all day?
- What is the best way to prevent malaria mosquito bites?
- What is the best mosquito repellent?
- How do I apply mosquito insect repellent?
- Where in the world is malaria found?
- Is malaria a contagious disease?
- What different types of malaria are there?
- How long after being bitten do symptoms occur?
- How do I know if I really have malaria?
- Are antimalarial drugs safe to use long term?
- Is it safe to buy my antimalarial drugs in the country where I will be travelling?
- Is there a malaria vaccine?
- What if I am pregnant?
- What if I am planning to get pregnant soon?
- If I am taking an antimalarial drug and breastfeeding, will my baby be protected?
- Can I take the contraceptive pill with my antimalarial medication?
- If I get malaria, will I have it for the rest of my life?
- Is malaria treatable?
- How can I prevent getting malaria?
- What are antimalarial drugs?
- Which antimalarial drug should I take?
- How long do I have to take antimalarial medicine for?
- What are the side effects of antimalarial medications?
- What are the cost differences of the antimalarial drugs?
- Do antimalarial tablets contain lactose or sucrose?
- Can I take homeopathy or herbal medicines to prevent malaria?
- Are some people immune to malaria?
- Does immunity to malaria reduce with time?
How do you get malaria?
People get malaria by being bitten by a mosquito infected with malaria parasites. When the mosquito feeds on blood from an infected human, the malaria parasites develop in the mosquito and mix with the mosquito's saliva. When the infected mosquito bites another person, malaria can be transmitted.
Because the malaria parasite lives in the red blood cells of an infected person, malaria can also be transmitted via blood transfusion, or the shared use of needles. Malaria may also be transmitted from a mother to her baby before or during delivery.
Do all mosquitoes transmit malaria?
No. Of over 2000 species of mosquito, only the female Anopheles mosquito transmits malaria. Male mosquitos don't bite. Females need protein for their eggs, and find it in blood.
The anopheles malaria mosquitoes are more likely to bite overnight between dusk and dawn. However other mosquitoes do bite during the day and they can carry other diseases such as Dengue fever, yellow fever, and Zika virus.
Are malaria mosquitoes active all day?
No, actually malaria transmitting mosquitoes feed mainly between sunset and sunrise, thus mosquito nets and repellent coils burning overnight are useful to prevent bites and malaria transmission.
What is the best way to prevent malaria mosquito bites?
Mosquitoes can bite at any time of day. Most bites by malaria mosquitos occur in the evening and overnight between dusk and dawn.
- Wear long-sleeved clothing and long trousers if you are out at dusk, dawn, and at night. Several companies sell insect resistant travel clothing pre-treated with insecticide (permethrin).
- Use insect repellent containing DEET on exposed skin and under thin clothing, particularly around the ankles. The best strength DEET is 50% There is no added benefit to using higher concentrations. Other repellents containing picaridin 20% or lemon eucalyptus 30% are less effective than DEET and must be reapplied very frequently.
- Insect repellent room sprays, mosquito coils, and heating insecticide impregnated tablets all reduce the risk of bites and should be used to kill mosquitoes in bedrooms before going to bed.
- Where possible sleep in screened rooms and use a mosquito net, preferably one impregnated with insecticide (permethrin). Mosquitoes are deterred by air conditioning but not fans.
Ultrasound devices, mobile phone apps, garlic, Vitamin B, marmite, homeopathic products, tonic water, alcohol, tea tree oil, and citronella DO NOT prevent bites.
For further information see Travel Health Pro - Insect and tick bite avoidance and NHS - Malaria.
What is the best mosquito repellent?
The best choice is DEET 50%. It can be used safely in most people including infants over 2 months, during pregnancy, and when breastfeeding. There is no added benefit to using higher concentrations. DEET should be reapplied as soon as mosquitoes begin to 'show interest' again. DEET has been used as an effective insect repellent for over 50 years and is used by 500 million people annually. DEET can damage plastics including watch straps, watch covers, plastic jewellery, and credit cards.
Other repellents containing picaridin, lemon eucalyptus, or IR3535, are less effective than DEET and must be reapplied much more frequently.
How do I apply mosquito insect repellent?
Apply your insect repellent to all areas of skin which are not covered by clothing. Apply carefully to avoid eyes and mouth, spray onto hands then rub on face.
If using sunscreen then apply that, before the insect repellent. The insect repellent may reduce the SPF protection of the sunscreen slightly. The insect repellent should be reapplied after swimming, sweating, or washing, and after reapplying sunscreen. If the mosquitoes begin to fly closer/show interest again, then reapply insect repellent. Keep DEET away from plastics as it may damage them, e.g. credit cards, phones, watches, or glasses.
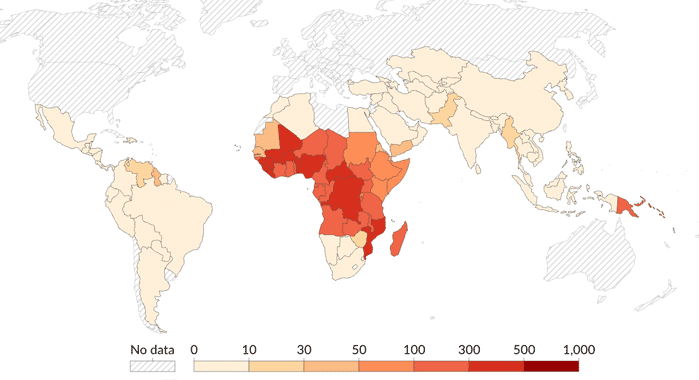
Where in the world is malaria found?
Malaria is found where the Anopheles mosquito thrives i.e. hot, wet climates. These are large areas of Africa and South Asia as well as Central and South America, also the Caribbean, Southeast Asia, the Middle East, Australasia/Oceania.
Is malaria a contagious disease?
No. Malaria cannot spread directly from person to person. It does not spread via the air like the flu, nor can it be sexually transmitted. Spread is only via infected blood, generally via mosquito bites.
What different types of malaria are there?
There are actually five different types of malaria caused by different plasmodium species. They are falciparum, vivax, ovale, malariae, and knowlesi.
Falciparum malaria is the most dangerous and most common causing 86% of UK cases in 2019.
The different types of malaria have slightly different life cycles, and so malaria symptoms can present up to a year after return from travel.
Malaria prevention medication works best against P.falciparum and P.vivax.
How long after being bitten do symptoms occur?
Usually between 1 week and 1 month, depending on the malarial strain.
P. Falciparum infection, which can be fatal, usually develops within a month and is very unlikely more than three months after the last possible exposure. It is found globally but most common in Africa.
P. vivax and P. ovale infection, while not fatal, can remain dormant in the liver for several months up to about 4 years, thus delaying onset of symptoms or causing relapses of malaria infection.
How do I know if I really have malaria?
Symptoms are similar to any flu-like illness including fever, shivers, sweating, backache, joint pains, headache, vomiting, diarrhoea, & sometimes delirium. Malaria is diagnosed by looking at your blood through a microscope (thick and thin films). If infected, parasites can be seen in the red blood cells. Self test kits (rapid diagnostic tests or dipsticks) are available for those travelling in remote areas away from medical care.
Are antimalarial drugs safe to use long term?
In general, the drugs used to prevent and treat malaria have been shown to be well tolerated for at least 1 year or more. The risk of developing malaria goes up the longer you stay in a malaria zone and so it is very important to continue antimalarial drugs. Detailed research studies have not been undertaken on long-term safety but the risk from contracting malaria is much greater. The UK malaria guidelines suggest that Malarone can be used for up to 1 year, doxycycline for up to 2 years, and Lariam for up to 3 years. This is outside the manufacturer's licence and doctors take responsibility for the prescribing. Some long-term travellers or expats rotate the antimalarial that they use each year.
Is it safe to buy my antimalarial drugs in the country where I will be travelling?
Medicines need to be started before you travel, and must be in-date. Buying medications abroad is risky. They could be of inferior quality, contaminated, or simply fake. Therefore they may not protect you against malaria and could be harmful. Dr Fox supplies genuine, UK licensed medicines, posted from a registered UK pharmacy.
Is there a malaria vaccine?
The search for an effective malaria vaccine is ongoing. Malaria vaccines have been developed and are being trialled in many African countries. However at present none are available for travellers and they are not as reliable as taking antimalarial tablets.
What if I am pregnant?
Pregnant women are at a much higher risk of being bitten, developing malaria, and becoming very seriously ill with a higher risk of death, of themselves or their unborn child, at any stage of pregnancy. Therefore, pregnant women are strongly advised not to travel to a malaria zone. If travel is completely unavoidable, they should take preventative medication and do all they can to avoid mosquito bites. They are more likely to be bitten as a pregnant woman's blood is very attractive to the malaria carrying mosquito. The insect repellent, DEET can be safely used up to 50% strength. DEET should not be swallowed and if breastfeeding, hands and breast skin should be washed before feeds.
What if I am planning to get pregnant soon?
The best option is to defer attempting to conceive until after the visit. Take the antimalarial of choice during your visit and wait for it to wash out of your system completely before conception.
| Antimalarial | Time to wait after last tablet until conception | ||
|---|---|---|---|
| Mefloquine (Lariam) | 3 months | ||
| Atovaquone/proguanil (Malarone) | 2 weeks | ||
| Doxycycline | 1 week |
If you cannot wait then consult an expert in travel medicine - mefloquine may be suggested after a careful assessment. The risks from malaria are much higher in pregnancy. It is important to protect yourself and your unborn child.
If I am taking an antimalarial drug and breastfeeding, will my baby be protected?
No. The amount of medicine in breast milk is unlikely to be enough to provide protection against malaria for the infant.
The breast-fed infant should take their own antimalarial medication as in malaria prevention for children guidance.
Doxycycline should not be taken by breastfeeding women.
Mefloquine can be used and seems to be safe whilst breastfeeding, although the manufacturer recommends avoiding mefloquine when breastfeeding. This is because of a lack of trial-based safety evidence.
Malarone (atovaquone/proguanil) can also be used whilst breastfeeding, but again there is no trial-based safety data available.
Dr Fox does not prescribe for breastfeeding women or under 18s. Please consult your own GP or a specialist in travel medicine.
Can I take the contraceptive pill with my antimalarial medication?
All the antimalarial medications (Lariam, doxycycline, Malarone) can be taken alongside the contraceptive pill, and other forms of contraception. It is important to continue your contraceptive use during time in a malaria zone. Also see above What if I am planning to get pregnant soon?
If I get malaria, will I have it for the rest of my life?
In general, no. With the right medications malaria is curable. The disease will continue if it is not treated or if it is treated with the wrong drug. Some medications are not effective because the parasite is resistant to them. That is why different drugs are sometimes recommended for different parts of the world.
In P. vivax and P. ovale malaria, the parasites can remain in the liver for several months up to about 4 years, thus delaying onset of symptoms or causing relapses of malaria infection as they reactivate.
P. malariae, if untreated, can stay in the blood for several decades.
Preventative malaria medication reduces but does not always completely prevent the development of malaria itself. Any malaria symptoms (fever, shivers, sweating, backache, joint pains, headache, vomiting, diarrhoea, cough) within a year of travel should be checked with a doctor.
Is malaria treatable?
Yes, the infection is curable, but it can be unpleasant to serious (including fatal). Prevention is better than cure.
How can I prevent getting malaria?
There are 2 ways:
- Avoid mosquito bites.
- Take antimalarial drugs, commonly Malarone, doxycycline and Lariam while you are in a malaria zone.
You should always use tablets AND bite avoidance.
What are antimalarial drugs?
These medicines are taken to prevent malaria: Malarone, doxycycline, Lariam.
They are started before entering a malaria zone and taken for varying lengths of time after leaving. They prevent the development of the malaria parasite within the body.
Which antimalarial drug should I take?
This depends on:
- Where you are going (the most appropriate antimalarial medication varies with location due to local resistance patterns). See travelhealthpro.org.uk.
- Any health issues you may have (as asked in the Dr Fox Pharmacy online consultation).
- Personal choice. The medicines have different regimes (how often and how long they need to be taken), different potential side effects, as well as different costs.
How long do I have to take antimalarial medicine for?
Malarone (atovaquone plus proguanil) has the simplest regime. The dose is one tablet a day taken once a day, starting only 1-2 days before you travel and for just 1 week after your trip.
Doxycycline has the most time consuming regime - take one tablet once a day, starting 2 days before your trip and continuing for 4 weeks after you get back.
Mefloquine (Lariam) has an easy regime. You only need to take one tablet weekly, starting 10 days to 3 weeks before the trip (so the treatment can be stopped and changed if you experience side effects) and for 4 weeks after you return.
What are the side effects of antimalarial medications?
Malarone (atovaquone plus proguanil) very rarely causes any side effects. When they do occur, tummy upsets and headache have been reported, also skin rash and mouth ulcers.
Doxycycline has possible side effects. Most common is that it can cause skin sensitivity to sunlight. As malarial areas are often sunny this can result in sunburn. Other side effects are stomach upset, indigestion, and thrush.
Mefloquine (Lariam) can have marked side effects affecting mental health and should be stopped if these occur. It is best avoided if you or a close family member have mental health problems. Other common side effects include headache, nausea, vomiting, and rashes.
More information about side effects is detailed in the medical information and the patient information leaflets included in medicine packs:
- Malarone (atovaquone/proguanil) patient leaflet
- Doxycycline 100mg Patient Leaflet
- Lariam Patient Leaflet
What are the cost differences of the antimalarial drugs?
Malarone (atovaquone plus proguanil) is expensive - the most expensive of the antimalarial tablets, so may be better for short trips. A non-branded generic cheaper version is also available.
Doxycycline is the lowest cost option.
Mefloquine (Lariam) is relatively cheap - not quite as cheap as doxycycline but cheaper than Malarone.
Please see current prices on the antimalarial tablets page.
Do antimalarial tablets contain lactose or sucrose?
Mefloquine (Lariam) contains lactose. Malarone and doxycycline do not contain lactose or sucrose.
Can I take homeopathy or herbal medicines to prevent malaria?
No. The Faculty for Homeopathy does not recommend using homeopathic medicines to prevent malaria.
The Health Protection Agency Advisory Committee on Malaria Prevention does not recommend relying on any herbal or homeopathic remedies for the prevention of malaria. They have not been tested and are not licensed, and there is no scientific proof supporting their use.
Choosing to rely on herbal or homeopathic malaria prevention is unlikely to be acceptable to travel insurance providers.
Are some people immune to malaria?
Partial 'acquired immunity' to malaria builds up in people who live in malaria areas who become repeatedly infected with malaria, often from a young age.
People who are carriers for sickle cell disease have some degree of protection from developing malaria. However those with sickle cell disease are at more serious risk of malaria.
It is still important to take antimalarial tablets, even if you think you have some immunity.
Does immunity to malaria reduce with time?
People, such as long-term immigrants to the UK, will lose any 'acquired immunity' rapidly when they are no longer living in malarious regions. Second generation who have not been born and brought up in a malaria region will have no acquired immunity.
Also previously non-malarious regions where immigrants lived before may also now have become malarious areas. When returning to visit relatives all former residents and their families will need to take antimalaria precautions.

Authored 29 October 2013 by Dr Tony Steele
MB ChB Sheffield University 1983. Former hospital doctor and GP. GMC no. 2825328
Reviewed by Dr A. Wood, Dr C. Pugh, Dr B. Babor
Last reviewed 08 September 2021
Last updated 28 October 2025


